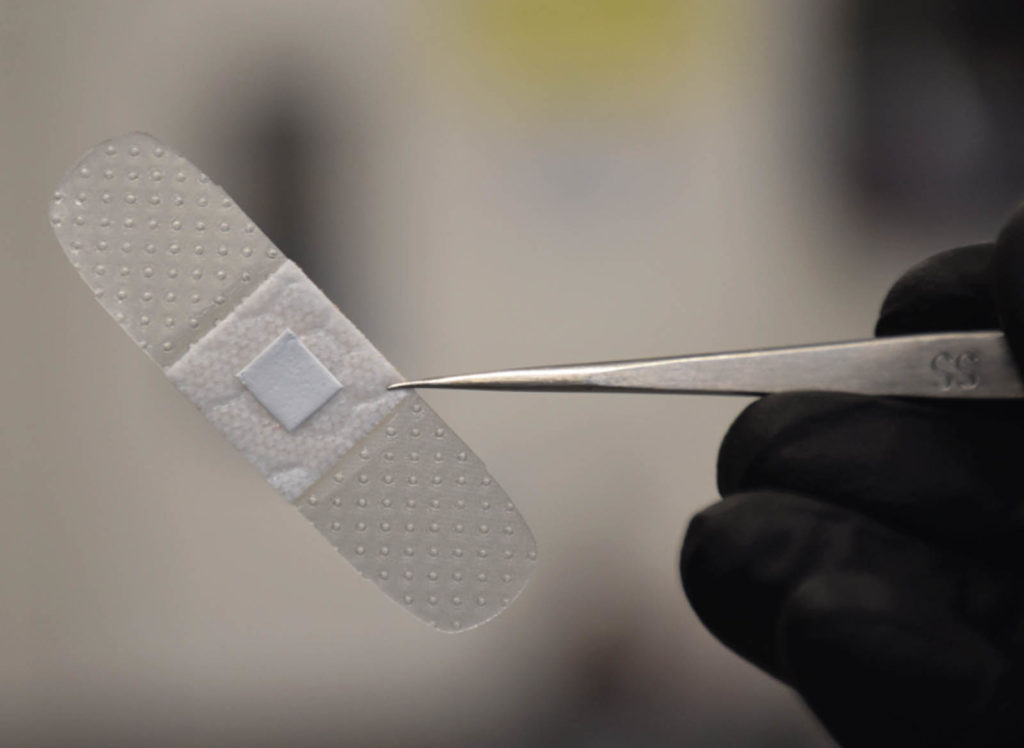
University of Rhode Island (URI) assistant professor Daniel Roxbury and former URI graduate student Mohammad Moein Safaee have created a continuous, noninvasive way to detect and monitor an infection in a wound by imbedding nanosensors in a “smart bandage.”
“Single-walled carbon nanotubes within the bandage will be able to identify an infection in the wound by detecting concentrations of hydrogen peroxide,” Roxbury says. Until now, the challenge with using nanotubes for this purpose has been immobilizing them in a biocompatible manner in such a way that they will stay sensitive to their surroundings.
“The microfibers that encapsulate the carbon nanotubes accomplish both of these tasks,” he says. “The nanotubes do not leach from the material, yet they stay sensitive to hydrogen peroxide within the wounds.”
The bandage will be monitored by a miniaturized wearable device, which will wirelessly (optically) detect the signal from the carbon nanotubes in the bandage. The signal can then be transmitted to a smartphone to alert the patient or a healthcare provider.
“This device will solely be used for diagnostic purposes,” he says. “However, the hope is that the device will diagnose an infection at an early stage, necessitating fewer antibiotics and preventing drastic measures, such as limb amputation. We envision this being particularly useful in those with diabetes, where the management of chronic wounds is routine.”
The next stage of the project will involve the verification that the bandages function properly in a petri dish with live cultured cells that would be found in wounds.
“The cells we will be using are known as fibroblasts and macrophages (white blood cells) that produce hydrogen peroxide in the presence of pathogenic bacteria,” says Roxbury. “If all goes well, we’ll move to ‘in vivo’ testing in mice. At that point, we would find a collaborator who specializes in these animal wound models.”
Testing has focused on small bandage samples, but the technology can be applied easily to much larger bandages. “There really is no limitation in terms of the size,” he says. “In fact, this technology will be most useful in large bandages.”
The technology behind the smart bandage is further described in an article published in Advanced Functional Materials. Roxbury, Safaee and URI doctoral student Mitchell Gravely authored the article.
 TEXTILES.ORG
TEXTILES.ORG


